
What is Spinal Stenosis? A PT’s Guide to the Definition, Causes, and Recovery
Most don’t think of Spinal Stenosis as a "functional diagnosis," but it is. Stenosis is the reduction of space within your spine—essentially "wrinkles on the inside." While it can appear on an MRI as arthritis or narrowing of the space in your spine, it really only becomes spinal stenosis when it becomes symptomatic. Whether you have central canal stenosis (affecting both legs) or foraminal/lateral stenosis (affecting one side), the key to a full recovery is to improve your body’s tissue tolerance. In my 10+ years of PT experience, I’ve found that focusing on what you can change—your strength, mobility, and nerve tolerance- is the path to pain-free living, even if your MRI stays the same.
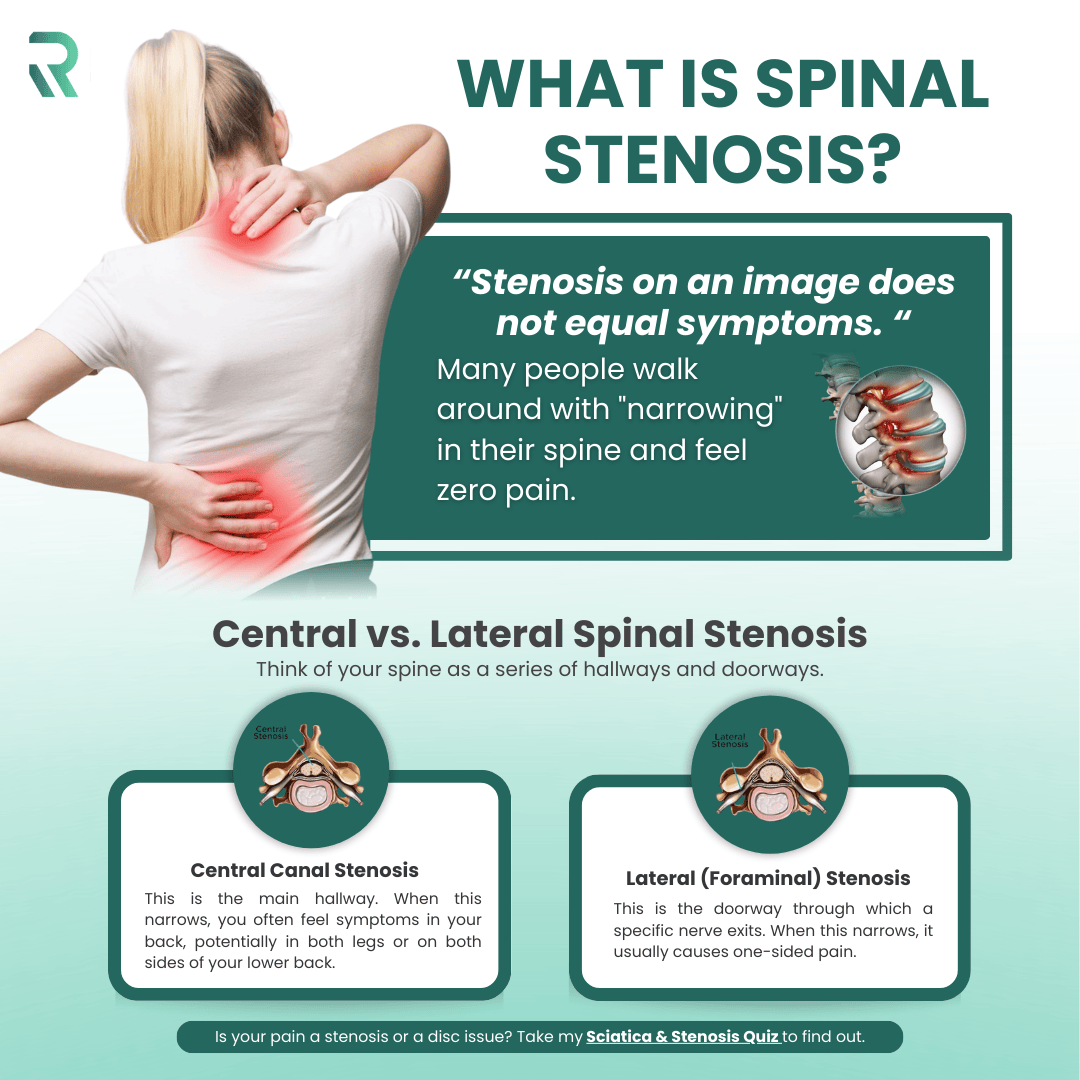
What is Spinal Stenosis? (The Definition)
When I treat patients, I often see patients who are terrified by their imaging results. Rightfully so, physicians usually don’t make you seem very good after receiving results. You know the word "stenosis" and think the worst. But here is the secret:
“Stenosis on an image does not equal symptoms. “
Many people walk around with "narrowing" in their spine and feel zero pain. Stenosis is simply a reduction of space caused by normal wear and tear. In treating thousands of patients, my definition of True Spinal Stenosis is that it becomes a real issue only when the space is so small that the nerves can no longer tolerate it.
Research indicates that for lumbar spinal stenosis, physical therapy and structured exercise programs provide similar long-term outcomes to surgery, with significantly fewer complications." (Zaina et al., 2016)
A landmark randomized trial comparing surgery to a structured PT program found no significant difference in outcomes at two years—meaning many patients can avoid surgery entirely by committing to the right rehabilitation approach (Delitto et al., 2015).
Central vs. Lateral Spinal Stenosis
Think of your spine as a series of hallways and doorways.
- Central Canal Stenosis: This is the main hallway. When this narrows, you often feel symptoms in your back, potentially in both legs or on both sides of your lower back. Again, primarily when you stand or walk.
- Lateral (Foraminal) Stenosis: This is the doorway through which a specific nerve exits. When this narrows, it usually causes one-sided pain.
What’s interesting about stenosis is that you don’t have to have a "line" of pain. I often see patients who only have calf pain, but the origin isn’t their leg—it’s coming from their back. If your calf hurts when you stand but feels better when you sit, spinal stenosis might be the culprit.
- Is your pain a stenosis or a disc issue? Take my Sciatica & Stenosis Quiz to find out.
Why "Wrinkles on the Inside" is the Better Way to Look at It
I encourage my patients to stop looking at their MRI as a broken or vulnerable spine and start looking at it as "wrinkles on the inside." Just as we get wrinkles on our skin or gray hair, our spines develop arthritis and space reduction over time. It’s a regular part of life. Early in the recovery process, we focus on what we can change (your movement) versus what we cannot (the arthritis). - We don’t need to, and you will learn this as well.
What Causes Spinal Stenosis?
When you stand or walk, you physically close off the space in your spine. If those tissues are already sensitive, they "complain." While these factors show up on your MRI, they don't have to cause any limitation or pain.
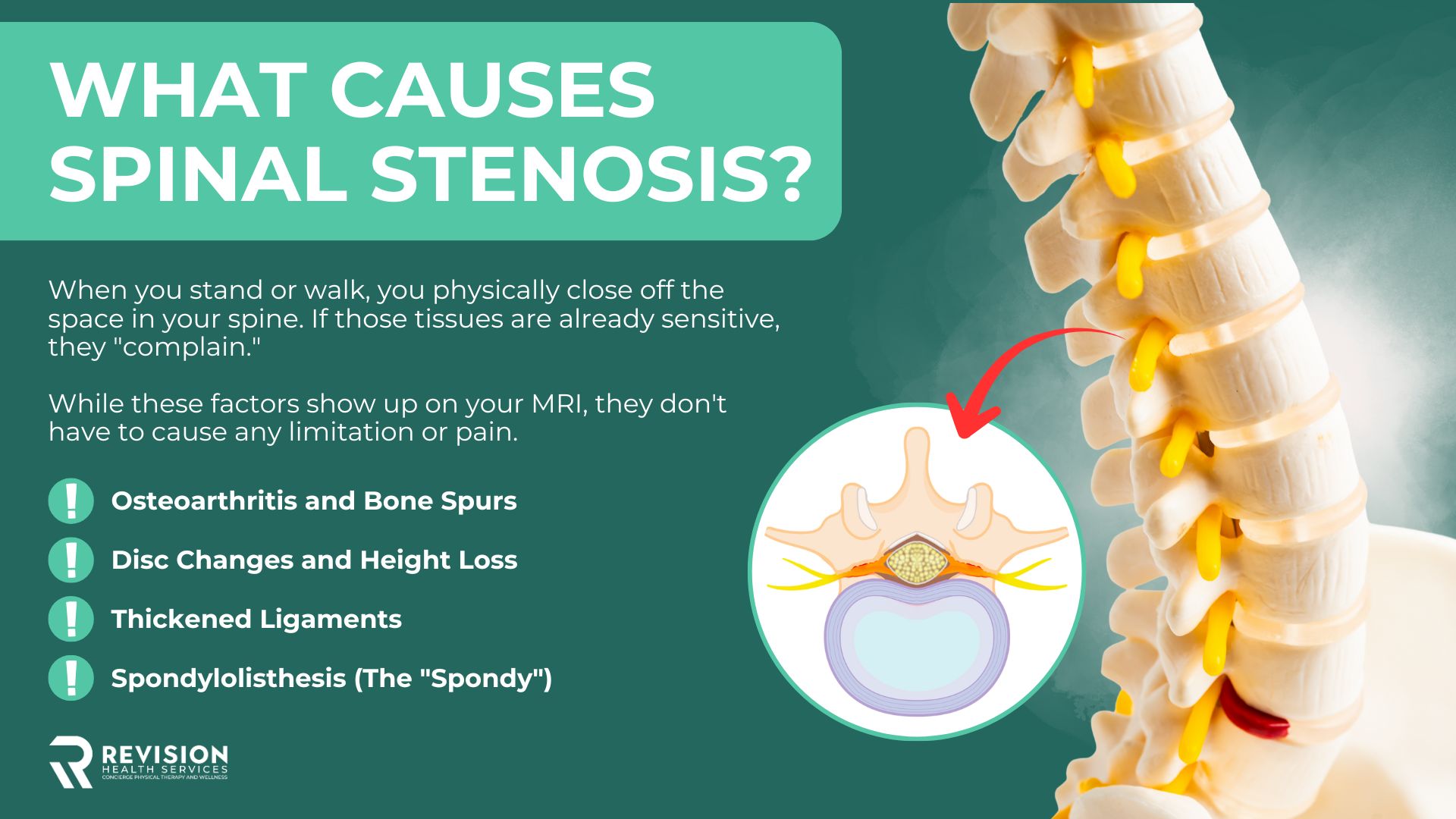
Osteoarthritis and Bone Spurs
As joints wear down, the body grows extra bone to create stability. Unfortunately, that extra bone can grow into spaces it shouldn’t be - stenosis.
Disc Changes and Height Loss
Over time, they lose fluid and "settle." This loss of height naturally reduces the space in the doorways where your nerves live. While disc herniations are very real, they often cause spinal stenosis, but they can also lead to sciatica.
Thickened Ligaments
The ligamentum flavum is a band of tissue in your spine. As we age, it can become thicker and less flexible, which takes up more space in the spinal canal.
Spondylolisthesis (The "Spondy")
This is when one vertebra slips slightly over another. While it sounds scary, you can achieve complete pain relief from a "spondy" without surgery by improving your tissue tolerance through skilled care. There are different grades of a spondy. Stage 1 to Stage 5.
Who Gets Spinal Stenosis? (Demographics & Risk Factors)
Is it Just Aging?
The most common demographic is adults aged 60 and older. This is simply because the "wrinkles" take time to develop, but they do grow. Remember, they don’t have to cause pain.
Risk Factors: From Genetics to Past Injuries
Some people are dealt a "crappy hand" with a naturally smaller spinal canal (genetics). However, a major overlooked risk factor is previous back surgeries or injuries. Surgeries or injuries create scar tissue, and over time, that scar tissue can take up the same precious space that the nerves need to breathe.
Can You Prevent Spinal Stenosis?
You can't prevent what they find on an image—age-related changes happen to everyone. But you can avoid the symptoms.
Loading the Spine Safely
Your spine needs to be loaded and is built to withstand load, so you must stay resilient. We teach you how to load it so that the nerves aren't irritated, but the bones and muscles stay strong.
Hip Mobility: The Secret to Relieving the Lower Back
If your hips are stiff, your lower back has to move more to compensate. By opening up your hips, you take the "pressure" off the narrowed areas of your spine.
Nourish the Nerves
The often missed part of recovery. The nerves in the spine are also becoming irritated, and you have to give them some specific attention. You can learn more here.
If you are the type of person who wants it all laid out for you—from hip mobility to spine strengthening—check out my Revision Sciatica Book. It is the comprehensive guide I wrote to help you move from fear to resiliency.
How to Recover: Reclaiming Your Walking Distance
Comprehensive recovery isn't about changing the MRI; it’s about understanding your symptoms and slowly progressing your strength. Walking with spinal stenosis can be especially challenging; to help overcome your walking difficulties, you could start here.
Learn about the Five Phases of Recovery for Spinal Stenosis on YouTube
Why "Flexion is Your Friend"
For almost everyone with stenosis, leaning forward (flexion) opens the "hallways." This is why you feel better leaning on a shopping cart. We use this principle to help you find relief so you can start exercising.
Building Core Resiliency (The Missing Link)
Recovery goes beyond basic ab or core exercises. It’s about "Core Resiliency"—teaching your body to support your spine during movement. Check out my new ebook on how to walk pain-free with spinal stenosis.

Your Next Steps to Reclaiming Your Movement
Step 1: Get Clarity. Stop guessing and start moving with a plan. Is your pain due to a disc issue or bony narrowing, such as stenosis? Take my free quiz to help figure precisely what you are dealing with and what your first move should be.
Step 2: Take Full Control. If you are tired of your legs feeling heavy and having to sit down every five minutes, my Pain-Free Walking Ebook is the solution. It’s the exact 4-phase system I use with my private clients to help them stand longer and walk farther with confidence.
Summary
Spinal stenosis isn’t a broken spine—it’s a functional condition where normal age-related “wrinkles on the inside” only matter if they create symptoms. An MRI showing narrowing doesn’t equal pain; symptoms happen when nerves lose tolerance, which is why many people with stenosis walk around pain-free. The path to recovery is focusing on what you can change, strength, mobility, and nerve tolerance, so you can live and walk pain-free even if your imaging never changes.
Most don’t think of Spinal Stenosis as a "functional diagnosis," but it is. Stenosis is the reduction of space within your spine—essentially "wrinkles on the inside." While it can appear on an MRI as arthritis or narrowing of the space in your spine, it really only becomes spinal stenosis when it becomes symptomatic. Whether you have central canal stenosis (affecting both legs) or foraminal/lateral stenosis (affecting one side), the key to a full recovery is to improve your body’s tissue tolerance. In my 10+ years of PT experience, I’ve found that focusing on what you can change—your strength, mobility, and nerve tolerance- is the path to pain-free living, even if your MRI stays the same.
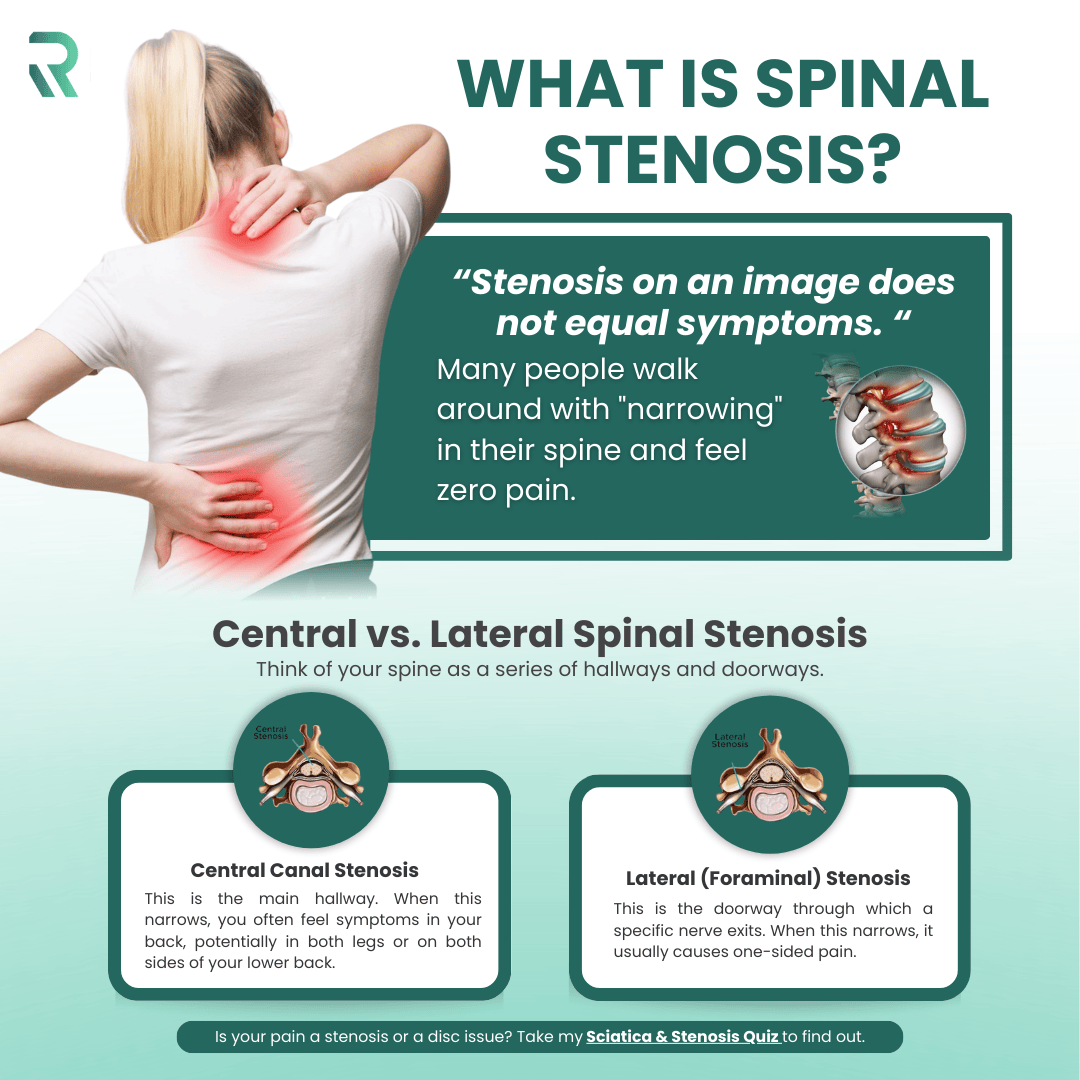
What is Spinal Stenosis? (The Definition)
When I treat patients, I often see patients who are terrified by their imaging results. Rightfully so, physicians usually don’t make you seem very good after receiving results. You know the word "stenosis" and think the worst. But here is the secret:
“Stenosis on an image does not equal symptoms. “
Many people walk around with "narrowing" in their spine and feel zero pain. Stenosis is simply a reduction of space caused by normal wear and tear. In treating thousands of patients, my definition of True Spinal Stenosis is that it becomes a real issue only when the space is so small that the nerves can no longer tolerate it.
Research indicates that for lumbar spinal stenosis, physical therapy and structured exercise programs provide similar long-term outcomes to surgery, with significantly fewer complications." (Zaina et al., 2016)
A landmark randomized trial comparing surgery to a structured PT program found no significant difference in outcomes at two years—meaning many patients can avoid surgery entirely by committing to the right rehabilitation approach (Delitto et al., 2015).
Central vs. Lateral Spinal Stenosis
Think of your spine as a series of hallways and doorways.
- Central Canal Stenosis: This is the main hallway. When this narrows, you often feel symptoms in your back, potentially in both legs or on both sides of your lower back. Again, primarily when you stand or walk.
- Lateral (Foraminal) Stenosis: This is the doorway through which a specific nerve exits. When this narrows, it usually causes one-sided pain.
What’s interesting about stenosis is that you don’t have to have a "line" of pain. I often see patients who only have calf pain, but the origin isn’t their leg—it’s coming from their back. If your calf hurts when you stand but feels better when you sit, spinal stenosis might be the culprit.
- Is your pain a stenosis or a disc issue? Take my Sciatica & Stenosis Quiz to find out.
Why "Wrinkles on the Inside" is the Better Way to Look at It
I encourage my patients to stop looking at their MRI as a broken or vulnerable spine and start looking at it as "wrinkles on the inside." Just as we get wrinkles on our skin or gray hair, our spines develop arthritis and space reduction over time. It’s a regular part of life. Early in the recovery process, we focus on what we can change (your movement) versus what we cannot (the arthritis). - We don’t need to, and you will learn this as well.
What Causes Spinal Stenosis?
When you stand or walk, you physically close off the space in your spine. If those tissues are already sensitive, they "complain." While these factors show up on your MRI, they don't have to cause any limitation or pain.
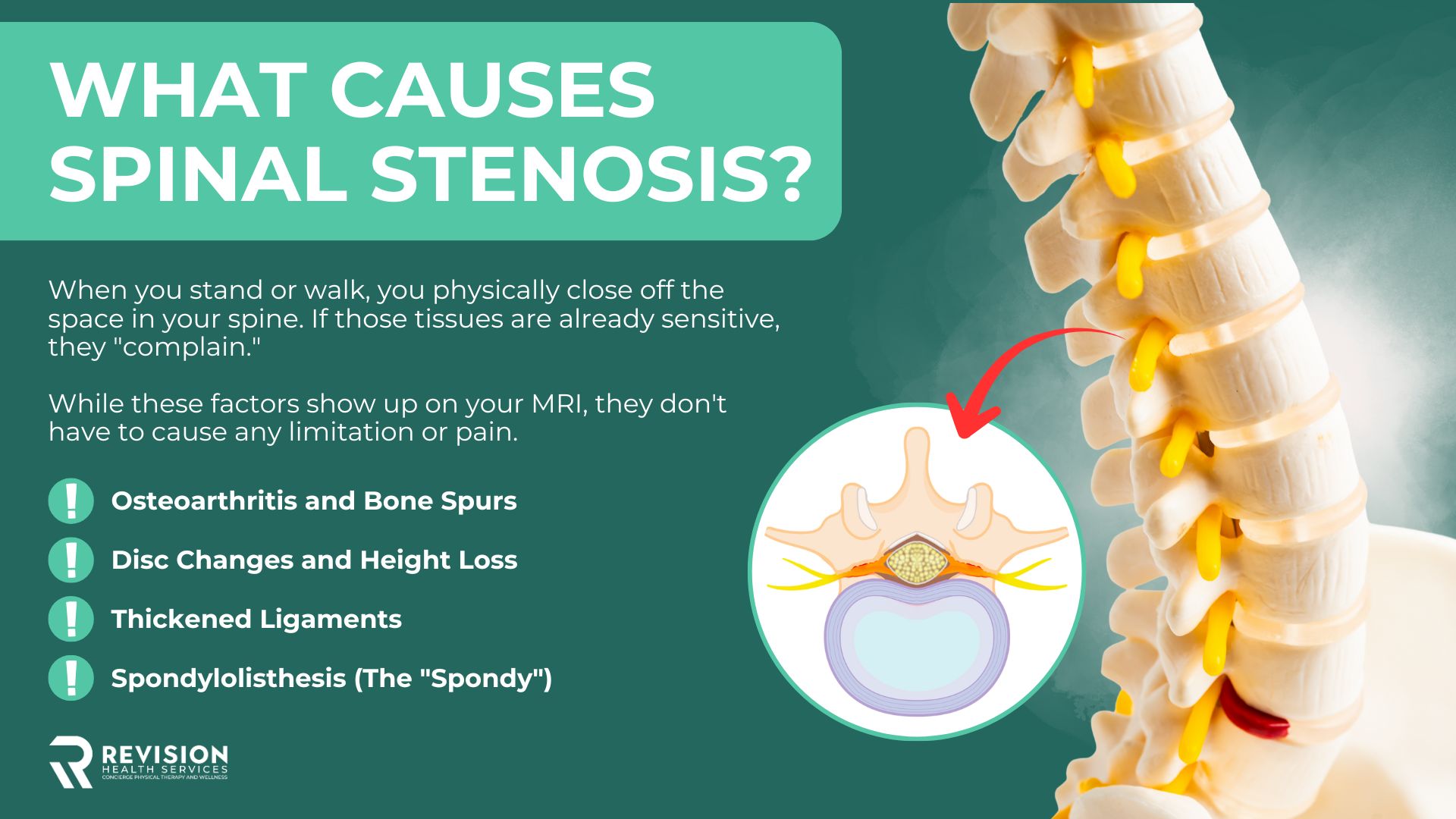
Osteoarthritis and Bone Spurs
As joints wear down, the body grows extra bone to create stability. Unfortunately, that extra bone can grow into spaces it shouldn’t be - stenosis.
Disc Changes and Height Loss
Over time, they lose fluid and "settle." This loss of height naturally reduces the space in the doorways where your nerves live. While disc herniations are very real, they often cause spinal stenosis, but they can also lead to sciatica.
Thickened Ligaments
The ligamentum flavum is a band of tissue in your spine. As we age, it can become thicker and less flexible, which takes up more space in the spinal canal.
Spondylolisthesis (The "Spondy")
This is when one vertebra slips slightly over another. While it sounds scary, you can achieve complete pain relief from a "spondy" without surgery by improving your tissue tolerance through skilled care. There are different grades of a spondy. Stage 1 to Stage 5.
Who Gets Spinal Stenosis? (Demographics & Risk Factors)
Is it Just Aging?
The most common demographic is adults aged 60 and older. This is simply because the "wrinkles" take time to develop, but they do grow. Remember, they don’t have to cause pain.
Risk Factors: From Genetics to Past Injuries
Some people are dealt a "crappy hand" with a naturally smaller spinal canal (genetics). However, a major overlooked risk factor is previous back surgeries or injuries. Surgeries or injuries create scar tissue, and over time, that scar tissue can take up the same precious space that the nerves need to breathe.
Can You Prevent Spinal Stenosis?
You can't prevent what they find on an image—age-related changes happen to everyone. But you can avoid the symptoms.
Loading the Spine Safely
Your spine needs to be loaded and is built to withstand load, so you must stay resilient. We teach you how to load it so that the nerves aren't irritated, but the bones and muscles stay strong.
Hip Mobility: The Secret to Relieving the Lower Back
If your hips are stiff, your lower back has to move more to compensate. By opening up your hips, you take the "pressure" off the narrowed areas of your spine.
Nourish the Nerves
The often missed part of recovery. The nerves in the spine are also becoming irritated, and you have to give them some specific attention. You can learn more here.
If you are the type of person who wants it all laid out for you—from hip mobility to spine strengthening—check out my Revision Sciatica Book. It is the comprehensive guide I wrote to help you move from fear to resiliency.
How to Recover: Reclaiming Your Walking Distance
Comprehensive recovery isn't about changing the MRI; it’s about understanding your symptoms and slowly progressing your strength. Walking with spinal stenosis can be especially challenging; to help overcome your walking difficulties, you could start here.
Learn about the Five Phases of Recovery for Spinal Stenosis on YouTube
Why "Flexion is Your Friend"
For almost everyone with stenosis, leaning forward (flexion) opens the "hallways." This is why you feel better leaning on a shopping cart. We use this principle to help you find relief so you can start exercising.
Building Core Resiliency (The Missing Link)
Recovery goes beyond basic ab or core exercises. It’s about "Core Resiliency"—teaching your body to support your spine during movement. Check out my new ebook on how to walk pain-free with spinal stenosis.

Your Next Steps to Reclaiming Your Movement
Step 1: Get Clarity. Stop guessing and start moving with a plan. Is your pain due to a disc issue or bony narrowing, such as stenosis? Take my free quiz to help figure precisely what you are dealing with and what your first move should be.
Step 2: Take Full Control. If you are tired of your legs feeling heavy and having to sit down every five minutes, my Pain-Free Walking Ebook is the solution. It’s the exact 4-phase system I use with my private clients to help them stand longer and walk farther with confidence.
Summary
Spinal stenosis isn’t a broken spine—it’s a functional condition where normal age-related “wrinkles on the inside” only matter if they create symptoms. An MRI showing narrowing doesn’t equal pain; symptoms happen when nerves lose tolerance, which is why many people with stenosis walk around pain-free. The path to recovery is focusing on what you can change, strength, mobility, and nerve tolerance, so you can live and walk pain-free even if your imaging never changes.
References
- Brinjikji, W., et al. (2015). Systematic Literature Review of Imaging Features of Spinal Degeneration in Asymptomatic Populations. AJNR. American Journal of Neuroradiology, 36(4), 811–816.
- Delitto, A., et al. (2015). Surgery versus nonsurgical treatment of lumbar spinal stenosis: a randomized trial. Annals of Internal Medicine, 162(7), 465–473.
- Zaina F, Tomkins-Lane C, Carragee E, Negrini S. Surgical versus non-surgical treatment for lumbar spinal stenosis. Cochrane Database Syst Rev. 2016 Jan 29;2016(1):CD010264.





