Types of Spinal Stenosis: Central vs Foraminal Lumbar Explained
If you’ve recently picked up your MRI report and saw words like "moderate central canal stenosis" or "severe neural foraminal narrowing," it’s completely normal to feel a surge of anxiety. Most medical reports don’t make us very hopeful for our bodies.
When I work with my clients in the clinic, the first thing I do is help them take a deep breath. Those scary words are often just "wrinkles on the inside." Just as we get wrinkles on our faces as we age, our spines change, too. These findings don't mean you are broken. In fact, most of the time, they show way more than necessary. – I hate this about MRIs.
In this blog, I’m going to break down exactly what these terms mean, why they cause different symptoms, and—most importantly—how we can improve your spine so you can get back to your life using a safe, consistent plan.
What Are the Different Types of Spinal Stenosis?
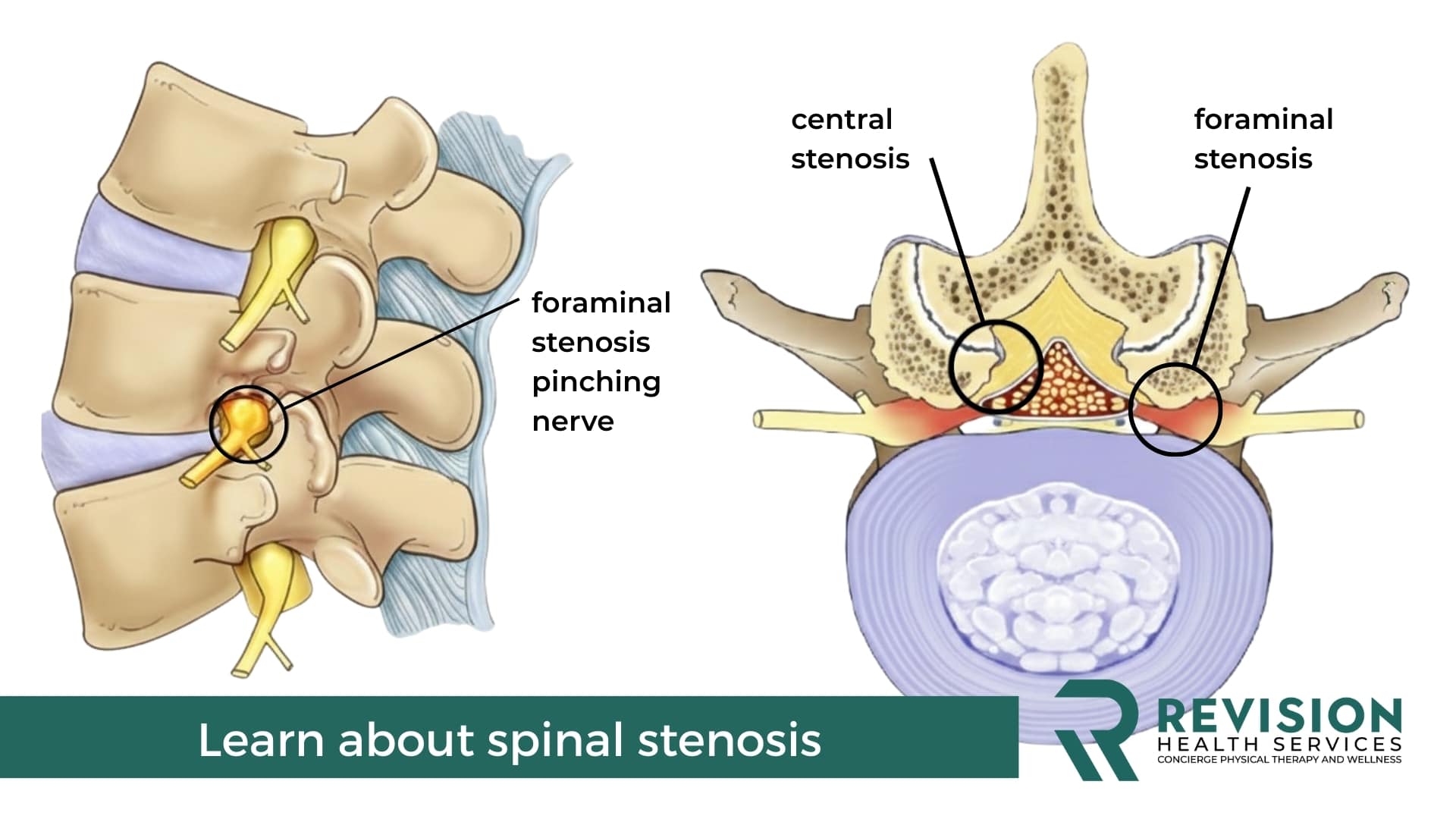
In simple terms, "stenosis" just means narrowing. Depending on where that narrowing happens, your symptoms and the way we treat them will change. To make this easier to visualize, imagine your spine as a large apartment building.
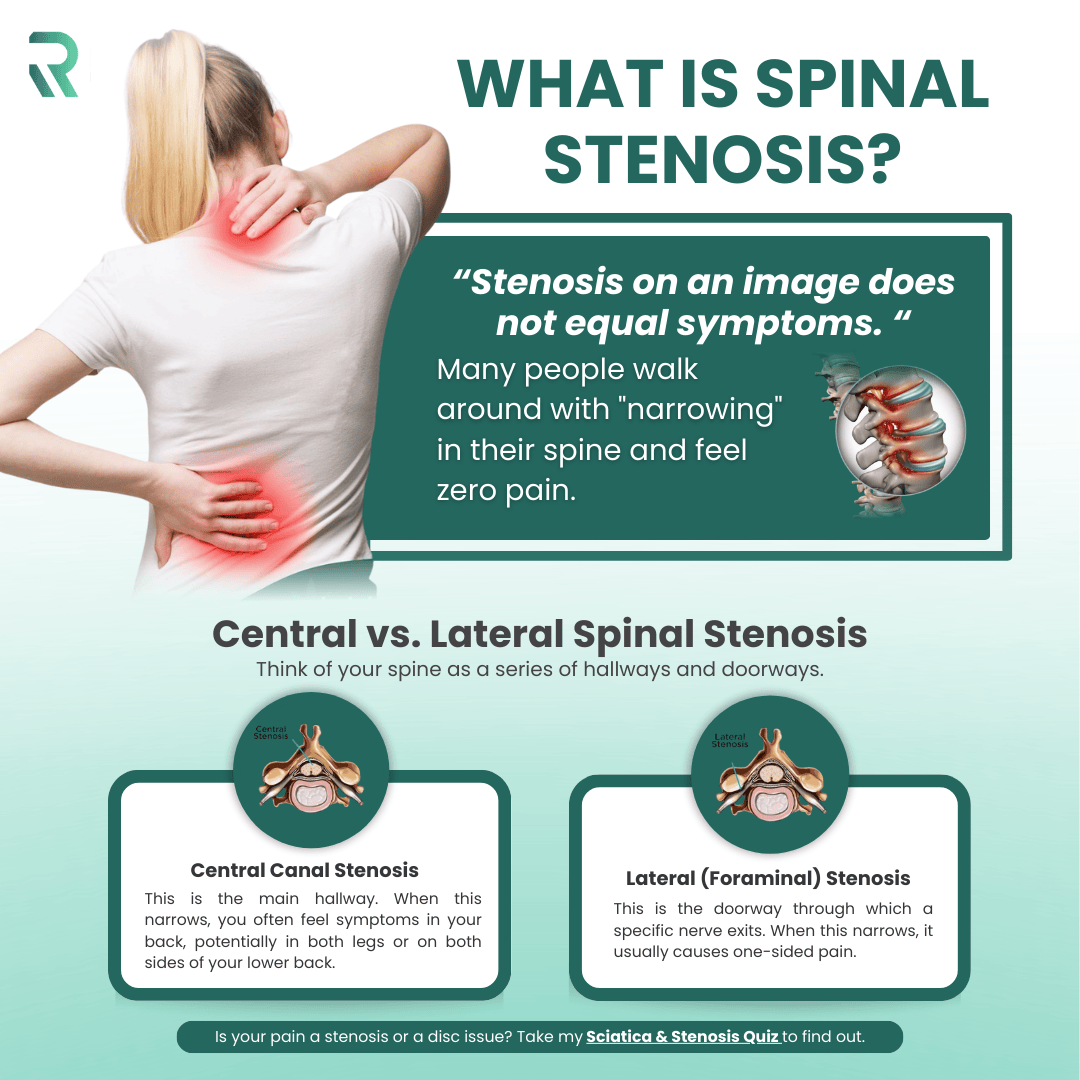
Central Canal Stenosis
Think of the Central Canal as the main hallway. This is the large opening in the middle of your vertebrae where the spinal cord (or the bundle of nerves called the cauda equina in your lower back) travels.
When you have Central Stenosis, the main hallway gets crowded. Because this affects the spinal cord the symptoms can show up in both legs. According to a PubMed study, central stenosis is most commonly caused by a combination of disc bulging, ligamentum flavum thickening, and facet joint arthritis (Genevay & Atlas, 2010). Which nearly all humans who are older than 50 have these findings. So, while common on an MRI, symptoms are way less common.
- What it feels like: Heaviness, cramping, or "lead legs" when walking or standing. Possibly numbness or tingling when you walk or stand for long periods of time
- Relief: You feel significantly better when leaning forward on a shopping cart or sitting down.
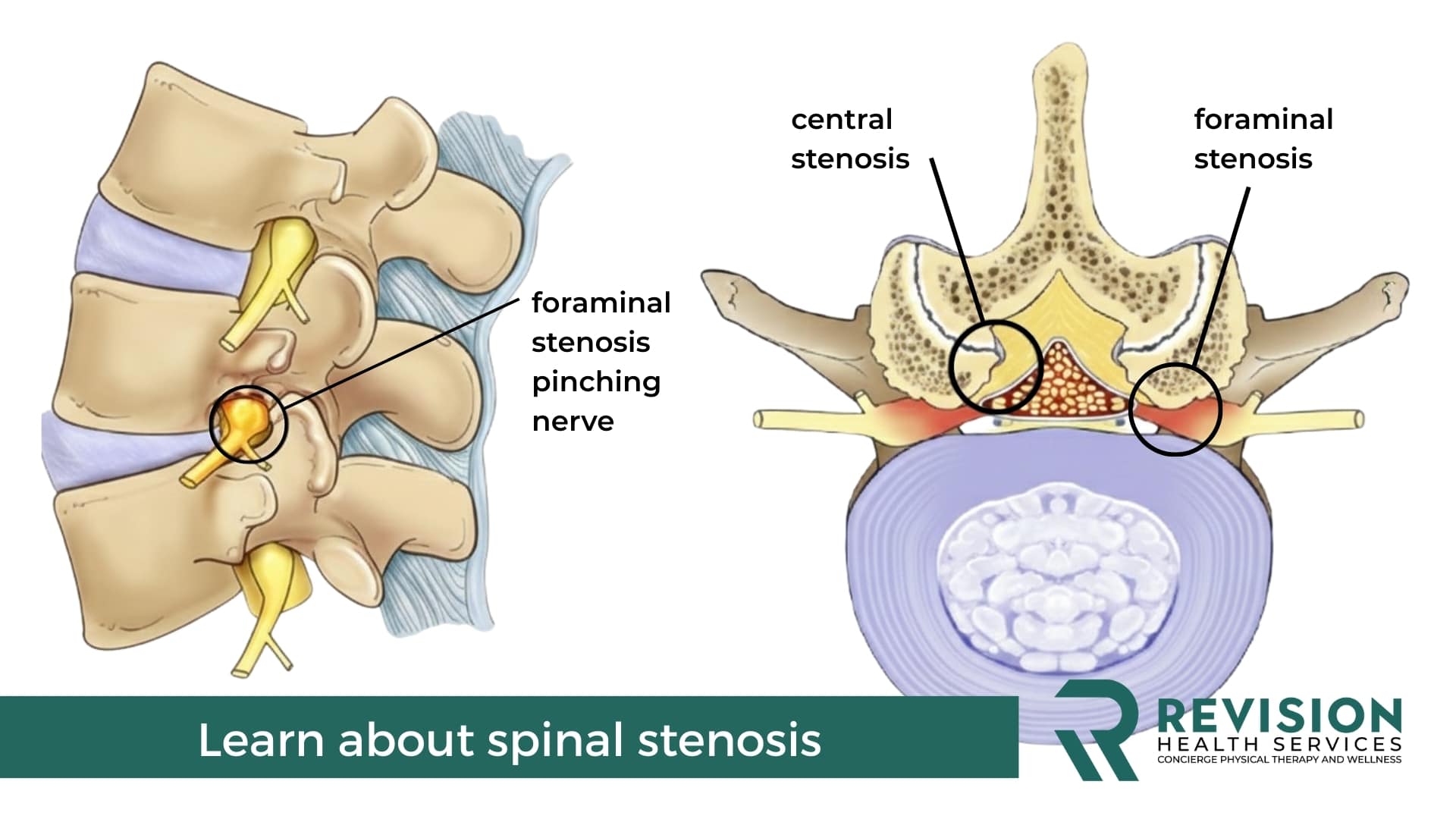
Foraminal Stenosis
Now, the individual nerves from your spinal cord need to leave to go to your legs. They exit through small side doors called the Foramina.
Foraminal Stenosis (often called neural foraminal narrowing) occurs when the foramen narrows. Unlike central stenosis, this usually affects just one side—the left or the right. I have seen this on an MRI as:
- Lateral foraminal stenosis
- Transforaminal stenosis
· What it feels like: Sharp, shooting pain, or "sciatica" down one leg.
This often mimics a herniated disc because it compresses a specific nerve root. If your report says "L4-L5 Foraminal Stenosis," it means the nerve exit at that specific level is a bit crowded. L4, L5, and S1 are the most common and often feel like sciatica. In fact, it can often cause sciatica.
If you are unsure if you have sciatica from stenosis, take this free quiz!
Neurogenic Claudication: The Walking Problem
The most common symptom I see with stenosis, which your doctor should see, is Neurogenic Claudication. I tell my patients to think of their nerves like a wet towel. They can take up fluid, but can’t really stretch when you pull them. Well, they get pulled like a wet towel and held like that so the water can’t get back in. That happens when you stand and walk, thus neurogenic claudication - nerve-like symptoms into the lower body when you stand or walk.
PubMed studies indicate that this happens because the narrowing restricts venous blood flow around the nerves (ischemia). When the nerves don't get enough blood, they start to tingle or feel heavy. This is not permanent damage! It is simply a signal that the nerve needs a "recharge." By leaning forward or sitting, you restore that blood flow immediately.
Walking is often the most limiting and painful symptom of stenosis. It can get better, but you must do it in a certain way. I recommend learning a lot about nerve glides, flexion exercises, and strengthening. Or, you can learn about all of those in my book: Revision Sciatica.
Lateral Recess Stenosis: The "In-Between" Space
If central is the hallway and Foraminal is the door, the Lateral Recess is the little "entryway" just before the door. Narrowing here is actually quite common at the L4-L5 level. It can cause a mix of symptoms—you might feel pain when standing, but it might only travel down one leg.
When I work with my patients, the exact name on the MRI matters less than how you move. Whether it’s the hallway, the entryway, or the door, our goal is the same: create space and improve nerve gliding.
Understanding L4-L5 and L5-S1 Findings
If you see these numbers, don't panic. L4-L5 and L5-S1 are the most common areas of wear and trear in the lower back. Research shows that these specific anatomical locations bear the most mechanical load, which is why "wrinkles" show up here first.
It is incredibly common to see "moderate stenosis" at these levels in people who have no pain at all. In my book, Revision Sciatica, I emphasize that we treat the human, not the image. We distinguish between the structural change (what the MRI sees) and your functional capacity (how you move).
L4-L5 and L5-S1 often cause sciatica. That can be pain into the leg, weakness, and tingling. It can be one of those or all of them. It's tricky and some think they have sciatica and they really don't. This video may help you figure this out!
The Solution: Stenosis Requires A Consistent and Safe Program
In Revision Sciatica I teach that the key to managing stenosis isn't a "quick fix" or a magic stretch. It’s about building a consistent and safe program that respects your nerves' current limits while slowly expanding them.
- Figure out the cause: We first identify the causue of the discomrot.
- Safely Strengthen: We focus on safe core and hip stability that supports the spine without forcing it into painful positions
- Consistency Over Intensity: Nerves thrive on repetitive, gentle movement (like nerve glides) rather than aggressive, heavy workouts.
- Tissue Tolerance: We are training your nerves to be less painful to movement.
Dr. Michael’s Pro-Tip: "The secret to long-term relief isn't doing 100 exercises once. It's doing 3 correct things consistently. My goal is to give you a plan that feels safe enough to do every single day."
Reclaim Your Body and Improve Your Pain
If you have tried some things on your own and want a structured, safe, and clinical approach:
The Revision Sciatica Book – This is my comprehensive guide to understanding your spine and implementing a consistent program that actually works for stenosis.
Pain-Free Walking eBook: Improve your walking with just 5 exercises and the exact guide that tells you what to do for the type of pain you may be feeling.
Summary
While these MRI findings can seem intimidating, remember that they are often a natural part of aging and do not define your physical potential. By focusing on a consistent, movement-based plan tailored to your specific type of narrowing, you can effectively manage these symptoms and regain your mobility. You are not "broken," and with the right approach, you can move past the discomfort towards a more active, confident lifestyle.
If you’ve recently picked up your MRI report and saw words like "moderate central canal stenosis" or "severe neural foraminal narrowing," it’s completely normal to feel a surge of anxiety. Most medical reports don’t make us very hopeful for our bodies.
When I work with my clients in the clinic, the first thing I do is help them take a deep breath. Those scary words are often just "wrinkles on the inside." Just as we get wrinkles on our faces as we age, our spines change, too. These findings don't mean you are broken. In fact, most of the time, they show way more than necessary. – I hate this about MRIs.
In this blog, I’m going to break down exactly what these terms mean, why they cause different symptoms, and—most importantly—how we can improve your spine so you can get back to your life using a safe, consistent plan.
What Are the Different Types of Spinal Stenosis?
In simple terms, "stenosis" just means narrowing. Depending on where that narrowing happens, your symptoms and the way we treat them will change. To make this easier to visualize, imagine your spine as a large apartment building.
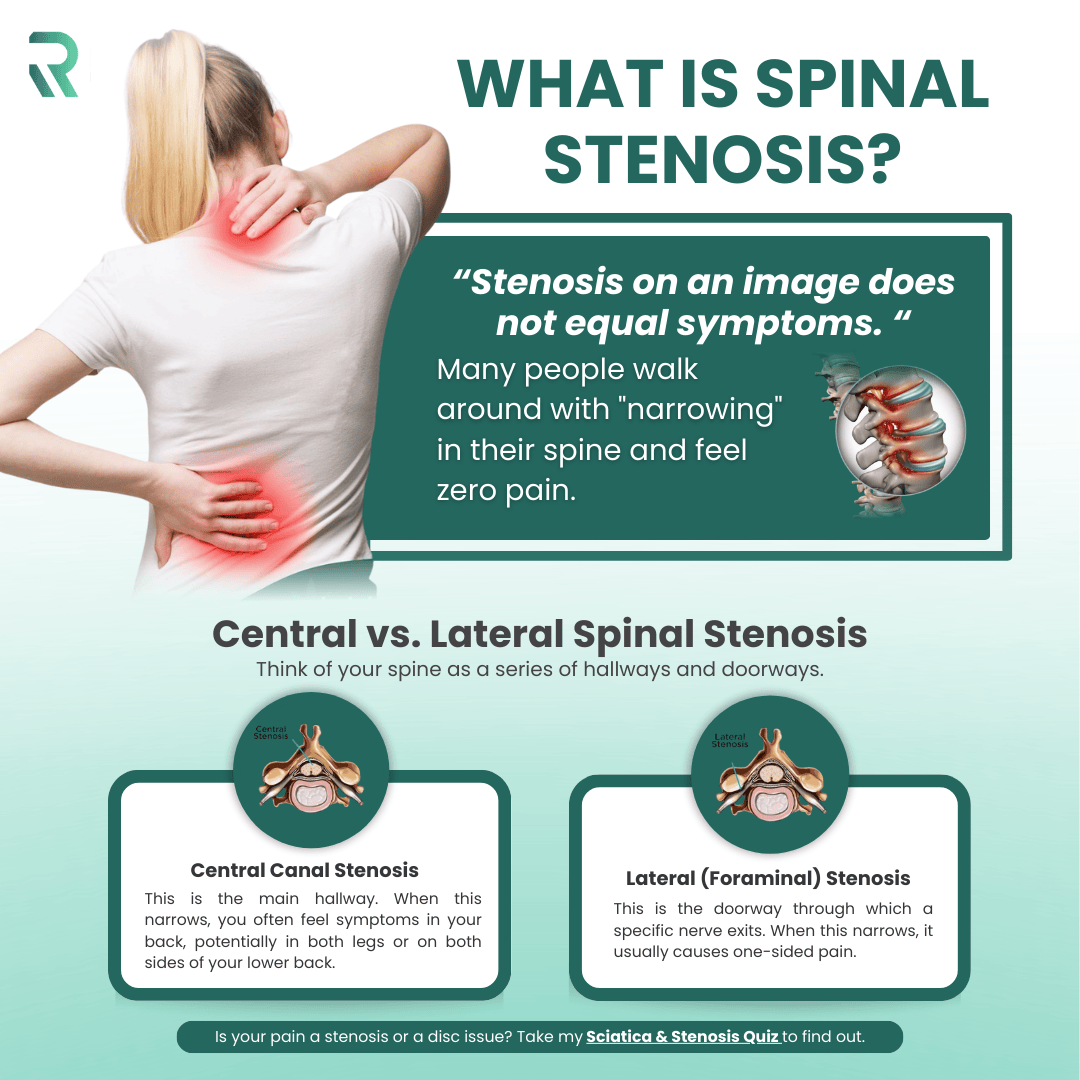
Central Canal Stenosis
Think of the Central Canal as the main hallway. This is the large opening in the middle of your vertebrae where the spinal cord (or the bundle of nerves called the cauda equina in your lower back) travels.
When you have Central Stenosis, the main hallway gets crowded. Because this affects the spinal cord the symptoms can show up in both legs. According to a PubMed study, central stenosis is most commonly caused by a combination of disc bulging, ligamentum flavum thickening, and facet joint arthritis (Genevay & Atlas, 2010). Which nearly all humans who are older than 50 have these findings. So, while common on an MRI, symptoms are way less common.
- What it feels like: Heaviness, cramping, or "lead legs" when walking or standing. Possibly numbness or tingling when you walk or stand for long periods of time
- Relief: You feel significantly better when leaning forward on a shopping cart or sitting down.
Foraminal Stenosis
Now, the individual nerves from your spinal cord need to leave to go to your legs. They exit through small side doors called the Foramina.
Foraminal Stenosis (often called neural foraminal narrowing) occurs when the foramen narrows. Unlike central stenosis, this usually affects just one side—the left or the right. I have seen this on an MRI as:
- Lateral foraminal stenosis
- Transforaminal stenosis
· What it feels like: Sharp, shooting pain, or "sciatica" down one leg.
This often mimics a herniated disc because it compresses a specific nerve root. If your report says "L4-L5 Foraminal Stenosis," it means the nerve exit at that specific level is a bit crowded. L4, L5, and S1 are the most common and often feel like sciatica. In fact, it can often cause sciatica.
If you are unsure if you have sciatica from stenosis, take this free quiz!
Neurogenic Claudication: The Walking Problem
The most common symptom I see with stenosis, which your doctor should see, is Neurogenic Claudication. I tell my patients to think of their nerves like a wet towel. They can take up fluid, but can’t really stretch when you pull them. Well, they get pulled like a wet towel and held like that so the water can’t get back in. That happens when you stand and walk, thus neurogenic claudication - nerve-like symptoms into the lower body when you stand or walk.
PubMed studies indicate that this happens because the narrowing restricts venous blood flow around the nerves (ischemia). When the nerves don't get enough blood, they start to tingle or feel heavy. This is not permanent damage! It is simply a signal that the nerve needs a "recharge." By leaning forward or sitting, you restore that blood flow immediately.
Walking is often the most limiting and painful symptom of stenosis. It can get better, but you must do it in a certain way. I recommend learning a lot about nerve glides, flexion exercises, and strengthening. Or, you can learn about all of those in my book: Revision Sciatica.
Lateral Recess Stenosis: The "In-Between" Space
If central is the hallway and Foraminal is the door, the Lateral Recess is the little "entryway" just before the door. Narrowing here is actually quite common at the L4-L5 level. It can cause a mix of symptoms—you might feel pain when standing, but it might only travel down one leg.
When I work with my patients, the exact name on the MRI matters less than how you move. Whether it’s the hallway, the entryway, or the door, our goal is the same: create space and improve nerve gliding.
Understanding L4-L5 and L5-S1 Findings
If you see these numbers, don't panic. L4-L5 and L5-S1 are the most common areas of wear and trear in the lower back. Research shows that these specific anatomical locations bear the most mechanical load, which is why "wrinkles" show up here first.
It is incredibly common to see "moderate stenosis" at these levels in people who have no pain at all. In my book, Revision Sciatica, I emphasize that we treat the human, not the image. We distinguish between the structural change (what the MRI sees) and your functional capacity (how you move).
L4-L5 and L5-S1 often cause sciatica. That can be pain into the leg, weakness, and tingling. It can be one of those or all of them. It's tricky and some think they have sciatica and they really don't. This video may help you figure this out!
The Solution: Stenosis Requires A Consistent and Safe Program
In Revision Sciatica I teach that the key to managing stenosis isn't a "quick fix" or a magic stretch. It’s about building a consistent and safe program that respects your nerves' current limits while slowly expanding them.
- Figure out the cause: We first identify the causue of the discomrot.
- Safely Strengthen: We focus on safe core and hip stability that supports the spine without forcing it into painful positions
- Consistency Over Intensity: Nerves thrive on repetitive, gentle movement (like nerve glides) rather than aggressive, heavy workouts.
- Tissue Tolerance: We are training your nerves to be less painful to movement.
Dr. Michael’s Pro-Tip: "The secret to long-term relief isn't doing 100 exercises once. It's doing 3 correct things consistently. My goal is to give you a plan that feels safe enough to do every single day."
Reclaim Your Body and Improve Your Pain
If you have tried some things on your own and want a structured, safe, and clinical approach:
The Revision Sciatica Book – This is my comprehensive guide to understanding your spine and implementing a consistent program that actually works for stenosis.
Pain-Free Walking eBook: Improve your walking with just 5 exercises and the exact guide that tells you what to do for the type of pain you may be feeling.
Summary
While these MRI findings can seem intimidating, remember that they are often a natural part of aging and do not define your physical potential. By focusing on a consistent, movement-based plan tailored to your specific type of narrowing, you can effectively manage these symptoms and regain your mobility. You are not "broken," and with the right approach, you can move past the discomfort towards a more active, confident lifestyle.